Epic’s Electronic Medical Record and Ancillary Systems Release AI Upgrades
Epic Systems announced a host of artificial intelligence (AI) tools last month at its annual conference. With its more than 300 million patient records (in a country with <400 million people) and more than 3500 different hospital customers, Epic has either released or is currently working on more than 200 different AI tools.1
Their vast data stores are being used to create predictive models and train their own AI tools. The scale of Epic and AI and what it can be used for is both exciting and frightening.
Optimizing Tools to Reduce the Burden of Health Care Administration
Typically, Epic Systems and other technology solution providers’ first entry into AI implementation comes in the form of reducing menial tasks and attempting to automate patient-customer interactions. In my discussions with health care administrators, it is not uncommon for them to attribute 40% to 60% of the cost of health care to administrative tasks or supports. For every physician, there are generally at least 3 full-time equivalencies (workforce members) needed to support that physician’s work, from scheduling to rooming patients to billing and a host of other support efforts.
About the Author
Troy Trygstad, PharmD, PhD, MBA, is the executive director of CPESN USA, a clinically integrated network of more than 3500 participating pharmacies. He received his PharmD and MBA degrees from Drake University and a PhD in pharmaceutical outcomes and policy from the University of North Carolina. He has recently served on the board of directors for the Pharmacy Quality Alliance and the American Pharmacists Association Foundation. He also proudly practiced in community pharmacies across the state of North Carolina for 17 years.
Reducing Cost and Improving Patient-Customer Experience
Reducing administration should reduce costs. Early-entry AI tools are generally aimed at reducing administrative cost, while simultaneously improving the patient experience extramural to the care delivery process (the bump in customer experience is the side benefit, not the motivation). In fact, all of us are more likely to be assigned an AI assistant as a customer than to use one as a health care provider at this juncture. AI is currently deployed over multiple sectors and customer service scenarios, interacting with us indirectly in recent years and now more directly as time passes. Remember that Siri and Alexa continue to grow just like humans, and now there are thousands and thousands of these AI bots. There is a strong possibility that if you answer a spam phone call, the “person” on the other end of the line is an AI tool (being?) and not a human.
Will AI Be an Antidote to Health Care Professional Burnout?
Charting is a drag. Ask any medical provider and one of their least favorite tasks is writing patient encounters for documentation’s sake rather than for the sake of patient care. I’ve personally known hundreds of physicians over my 2 decades of collaborating with them and the majority do most of their charting during off hours (thanks to technology), eating into their work-life balance and wellbeing. A recent study of providers using AI tools for charting found a 40% reduction in documentation burden and better and more complete charting.2 Could AI reduce the burden of menial pharmacy tasks that take away from patient care as well? Very likely yes.
But what if the business model doesn’t change? The biggest lie ever told in pharmacy was that technology was going to free pharmacists to provide patient care without a subsequent workflow and economic model to support it. Therefore, our profession went from filling 150 prescriptions a day to 300 a day to, in some cases, up to 500 per day per pharmacist. The only thing the technology did was increase the throughput of the existing business model. It didn’t support a new model at all.
That is the concern of many physicians as well. Will AI merely increase the number of encounters expected of them or will it actually improve their care delivery and practice satisfaction? That’s a question explored in a recent Harvard Business School article that points to upcoding bias (documentation of higher levels of care to bill more revenue), reduction in administrative cost, and reduced clerical full-time equivalents as the seeming “wins” for health systems administrators thus far, rather than better and more cost-efficient care delivery overall.3 Unsurprisingly to pharmacists, the business model is driving AI use, not the desired practice model.
AI as the New “Peripheral Brain” and Decision Support System
Those of us of a certain age remember a time in pharmacy school when we first entered the practice world under the supervision of a preceptor. At that time, the “peripheral brain” was a notebook that contained the latest prescribing guidelines, infectious disease–drug matches, and other clinical information. Then along came a handheld electronic version of it. Then came Google. Then the implementation of cloud computing. And now AI.
AI is already in place for many physicians and other health care providers, and I fear pharmacy may actually be late to the game in an arms race to make the drug assessment–prescribing–filling process even more efficient. But efficient at what? Administrative tasks? Order entry? Prior authorization documentation?
What About the Effects on Health System and Community Pharmacy Practice?
What if the rest of the world views the practice of pharmacy as consisting entirely of administrative tasks and not assessment and care delivery? If the AI tool is the physician’s peripheral brain, why is there a need for the pharmacist to make recommendations or find drug therapy problems? If the AI tool is instructing the care manager on which medications the care team needs to gather information about and report back to the peripheral brain, why have a pharmacist on the team? There will be many who say, “Oh, AI will absolutely replace the need for pharmacists because they don’t (actually) deliver care. They are a means of medication distribution and a great source of knowledge of medications, but AI will be better at that.”
Too Little Discussion and Planning Not Underway in Pharmacy Circles
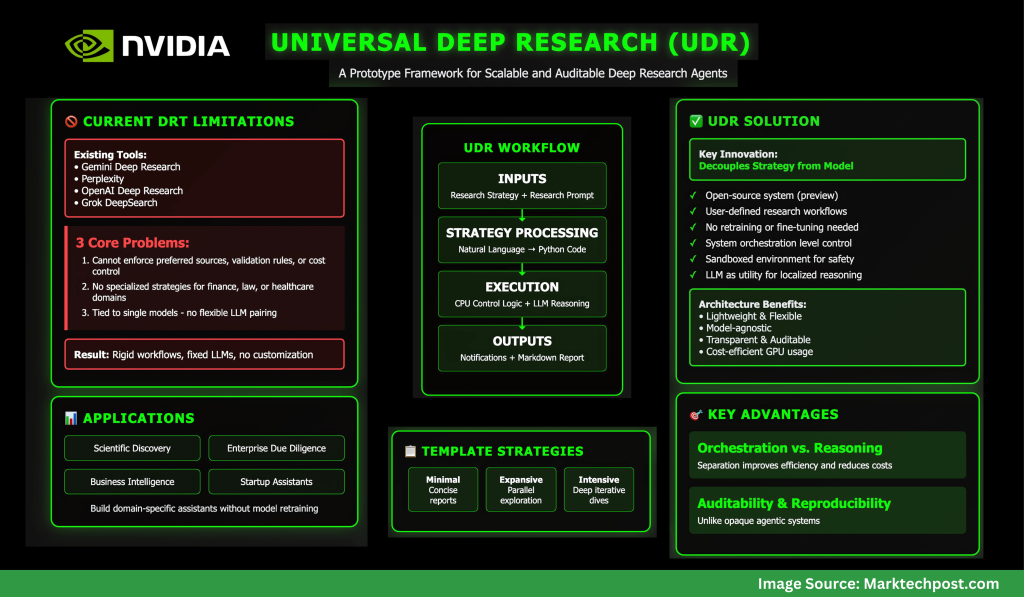
The AI takeover is not some distant future reality. The reality is weeks and months away, not years and decades. Nvidia (the chipmaker essential for AI processing) has seen its stock price rise more than 900% in the past 3 years as investors awaken to the speed with which AI is moving. AI is already starting to move from helper to replacement for many jobs and we could see AI agents doing research autonomously within 6 to 18 months and becoming the experts in every field of study known to humans by 2030 (or sooner).
What are we doing in the pharmacy world to prepare, take advantage of, and plant our flag as the medication optimization experts that utilize AI better than anyone else? As far as I can tell at this juncture, we’ve given AI a passing glance and are waiting for AI to come to us, rather than aligning and integrating with AI at the outset.
AI Could Be the Best and Worst Thing for Pharmacy. We Must Learn Lessons From the Past.
There is so much work to do, from regulatory discussions with our state boards of pharmacy to scoping the future of practice alongside technology solution providers to teaching the next generation of pharmacists as well as those already in practice about how to use AI to deliver safer, more effective, and more innovative care.
And above all, practice follows the business model. If provider status was important pre-AI, it has become critical post AI. If we are a profession of clerical work, we will be replaced. If we are a profession of providers, we will harness the immense capabilities of our future AI assistants. No more “This will save you time so you can care for patients” baloney, when there is no economic support model for care delivery sizable enough to employ a quarter of a million pharmacists. We should all be demanding to see evidence of the billable time from our employers, policy makers, and regulators. That is the only sustainable path when the peripheral brain is in the cloud and is the known universe’s best version of it.
REFERENCES
1. What health care provisions of the One Big Beautiful Bill Act mean for states. National Academy for State Health Policy. July 8, 2025. Accessed July 21, 2025. https://nashp.org/what-health-care-provisions-of-the-one-big-beautiful-bill-act-mean-for-states/
2. Graham J. The big, beautiful health care squeeze is here: what that means for your coverage. Investor’s Business Daily. July 18, 2025. Accessed July 21, 2025. https://www.investors.com/news/big-beautiful-bill-trump-budget-health-care-coverage/
3. Constantino AK. Bristol Myers Squibb, Pfizer to sell blockbuster blood thinner Eliquis at 40% discount. CNBC. July 17, 2025. Accessed July 21, 2025. https://www.cnbc.com/2025/07/17/bristol-myers-squibb-pfizer-to-sell-eliquis-at-40percent-discount.html